By Robyn Spizman Gerson –
Lauren Spanjer Bricks and the company she co-owns is at the forefront of COVID-19 testing. Bricks is chief operating officer of Ipsum Diagnostics in Sandy Springs, an independent medical laboratory that is one of only 12 with authorization from the Food and Drug Administration for COVID-19 molecular testing.
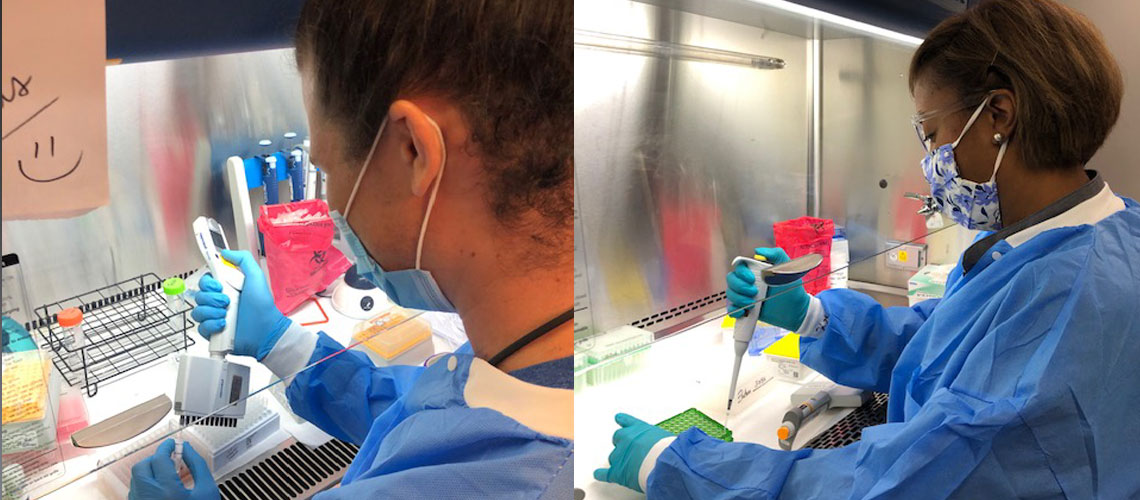
Ipsum’s lab is open around the clock and is testing thousands of COVID-19 samples per day with a 24-hour turnaround time. Bricks led her company of 100 employees to develop fast and accurate COVID-19 tests, helping to expand testing in Georgia. Founded in 2016, Ipsum specializes in clinical and anatomical testing services.
On April 1, the FDA granted emergency use authorization for the Ipsum Diagnostics COVID-19 test. Bricks and her team quickly recognized that Ipsum could adapt and share their test methodology to support other small, independent labs across the U.S. They worked with Mercer University Medical School, which is now operating Ipsum’s satellite laboratory, and helped bring testing to areas that had no COVID-19 testing.
The Atlanta native on the cutting edge of lifesaving testing is a 2005 University of Maryland graduate with a degree in biology and a Master of Business Administration. She has nearly a decade of experience in the realm of lab testing and lab diagnostics. “Atlanta is very important to me and my husband; we both grew up in Sandy Springs. My mother-in-law and her siblings were all born and raised here. I went to Riverwood High School, met my husband here in Atlanta,” Bricks said. “We live and work in Sandy Springs, both owning our own businesses that are close to home and The Davis Academy, where our children attend school.”
Dr. Steven Marlowe, infectious disease doctor and chief medical officer of Ipsum Diagnostics, said, “Our COVID-19 test, like all PCR (polymerase chain reaction) reference laboratory tests, is a snapshot in time. It is the best way to know if you are carrying the COVID-19 virus. A negative test, in general, means you are not infected with the virus at that particular moment. It does not predict the future. You could get infected right after you have a negative test,” Marlow stressed.
“Ideally everyone should be tested to prevent the spread of the virus. Currently, using CDC estimates, 94 percent of those tests would be negative. Realistically, we cannot now test the entire population. We have to do what epidemiologists call ‘stratify the risk” and rank by importance of the risk of infection.”
He offered some tips for when to get tested:
• If you have symptoms, talk with your primary care clinician. It is generally a good idea to get tested to confirm your diagnosis. He/she will make the decision with you based on your individual situation.
• You may need two negative tests at the end of your illness as a ‘proof of cure’ to go back to work.
• If you have a significant exposure and have no symptoms, self-quarantine and get tested in 14 days or later to make sure you’re not carrying the virus.
• Get tested periodically if you live or work in a high risk area.
• When planning to visit a highrisk family member or friend, get tested 24 hours prior to make sure you don’t infect them.
Marlowe added, “There is a lot of confusion about the time period of infection and when to get tested. The incubation period of COVID-19 is generally up to 14 days. That means if you are going to get sick (i.e. develop symptoms) you will know within 14 days after the exposure. Most people know in about five days. However, not everyone gets sick after getting infected.
“The CDC estimates 40 percent of people remain asymptomatic following infection. Those individuals carry the virus unknowingly and can infect others. That is presently the major reason why this pandemic is so difficult to contain. The best way to know if you are an asymptomatic carrier and unwittingly spreading the virus to others is to get a PCR test.”
The Sandy Springs lab is now expanding its testing. Bricks explained, “PCR testing is the most sensitive testing to detect the presence of the COVID-19 virus. It is based on finding minute amounts of a piece of the virus’ genetic code (RNA). What makes this testing method so unique is that it is designed for labs that are equipped to run a large volume of test samples in one session. Currently, our lab tests 7,000 samples per day. Furthermore, Ipsum can designate other laboratories to perform our test, and we are helping to expand testing in other communities around the country.”
Ipsum’s work is important, she said, beyond identifying those that need to be quarantined. Each patient has a different important reason for testing: reuniting a newborn with his mother who spiked a fever after delivery; employees able to go back to work; a cancer patient who can be cleared to have treatment, alleviating the nervousness and anxiety of not knowing, along with other critical challenges during the pandemic.
When asked about ramping up testing after the FDA granted authorization, Bricks said, “The hard part swiftly followed. The entire supply chain was disrupted. We had developed the paperless COVID portal where orders could be entered, created aggregate reports that would compile all positive reports into one file to
make reporting to different state
health departments simple, provided metrics on positivity rates, turnaround time, and had many other well thought out solutions to make the entire process seamless,” she said.
“What we hadn’t prepared for was that there
would be no swabs and all the basic lab consumables would be a challenge to procure. I never in my life thought I would be up all night stressed out over a swab. We had to come up with solutions. We found swabs, but there were no transport tubes available. We found a solution. The lab added 24/7 kit production assembly. We had ‘clean rooms’ and sterilization capabilities, we could make our own kits and put quality measures into place. We were able to provide the state with the collection kits they needed, going up every single week: 12,000, 25,0000, 35,0000 then 65,000.”
Bricks and her team were innovative in their approach to forging forward with their own FDA EUA. Not only did they develop the test, they came up with a userfriendly portal for patients and providers, and she was also the first to cater to the Spanish-speaking community by offering the test report in Spanish.
She said her goal is to help save as many lives as possible because everyone deserves to have access to fast and accurate medical testing.
“Testing is a keystone to controlling and conquering the COVID-19 pandemic. Pending the discovery of more effective treatments and vaccines, it is the best way to stop the spread. Only by testing and identifying cases can we isolate and quarantine people and break the transmission chain,” Bricks said. “Given the extent of the worldwide pandemic, most experts feel COVID-19 will be with us for quite a while. More technology and innovation are being done in our industry and we are hopeful for future progress.
Bricks added, “I am very proud that as a small lab we can accomplish significant feats.”